|
|
| Postmenopausal Endometrium |
|
Dr. Sharda Jain
Chairman,
Global Institute of Gynaecology
At Pushpanjali Crosslay Hoapital |
| Menopause sets in after 12 months of spontaneous amenorrhea amenorrhea. Mean age of menopause is 51 years. For a period varying from months to years before menopause, the individual patient may experience irregular patterns of bleeding. Often the first sign ia a shortening of the menstrual interval secondary to premature elevation in FHS, followed by intermittent periods of amenorrhea alternating with heavy bleeding consistent with oligoovulation or anovulation. With this clinical picture, special consideration must be given to ruling out a neoplastic process as the source of the heavy bleeding. The first consideration is to ensure that the bleeding originates from the uterus. In elderly women especially, bleeding from the urethra or rectum may be reported as vaginal bleeding. Vaginal cervical lesions causing the bleeding should be diagnosed readily with careful inspection or biopsy. Cancers of the vagina or cervix or cervical polyps can also be readily diagnosed and appropriate treatment rendered. |
 |
When the source of the bleeding is determined to be the uterine cavity, sampling of the endometrium for pathology examination is usually considered to be mandatory. Although D & C continues to be a commonly performed procedure for both its diagnostic and therapeutic benefits, office endometrial biopsy can often expedite appropriate evaluation and therapy. It has already replaced conventional D & C in 95% cases in western world.
Vacuum suction curettage has gained some popularity as an office procedure for endometrial sampling that does not require general anesthesia (probet endometrial curette)
World over office endometrial biopsy is almost 98% accurate in evaluating high-risk women with abnormal bleeding for endometrial malignant disease.
If the cause of postmenopausal bleeding is not identified in a screening endometrial biopsy, however, then a standard curettage is obligatory. In office biopsies of the endometrial of more than 20,000 patients of all ages, Hofmeister detected 273 cases of endometrial carcinoma, 32 of which (14.28%) were totally asymptomatic (2005).
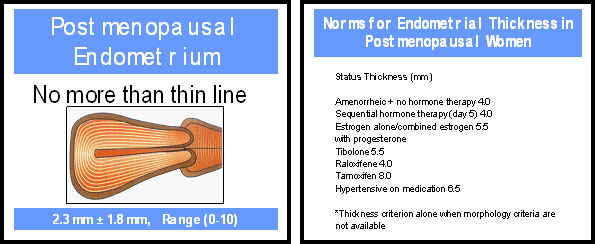
Vaginal ultrasound has been investigated as a screening tool in patient with postmenopausal bleeding. The average thickness of the postmenopausal endometrial stripe has been reported as 2.3 ± 1.8 mm, with a range of 0 to 10 mm, in a series of 300 asymptomatic women. Twenty-two had endometrial stripes of 5 mm or larger, and all had benign pathology.
In a series of 50 cases of postmenopausal bleeding , Nasri and colleagues from middle east reported that if the endometrial thickness was less than 5 mm, the pathology would show either inactive or no endometrial tissue. However, no body can be 100% sure of excluding malignanct pathology. Review of literature show that an endometrial echo of less than 4 mm had a sensitivity of 96% and a specificity of 68% for detecting endometrial pathology in postmenopausal patient. Sensitivity is the probability of testing positive if the disease is truly present. Specificity is the probability of testing negative if the disease is truly absent.
A metaanalysis reviewing the accuracy of transvaginal sonography reported that 96% of women with endometrial cancer and 92% of women with other endometrial diseases like polyps if an endometrial echo of greater than 5 mm (Smith-Bindman et al).
Saline infusion sonography (SIS) can be used to further evaluate patients with thickened endometrial stripes to detect structural problems such as polyps as an adjunct to endometrial sampling.
Office hysteroscopy using new smaller diameter flexible or rigid hysteroscopes is growing in popularity because it enables selective biopsy of the areas of visualized endometrium that appear most likely to contain a neoplastic process. We all know that a neoplastic transformation in the endometrium is often a focal abnormality. Another major advantage of hysteroscopy is the diagnosis of endometrial polyps, submucous myomas, or other source of bleeding that may not always be identified by endometrial biopsy or conventional curettage.
It is not uncommon to obtain no tissue from patients with marked hypertension or from patients undergoing chronic anticoagulant therapy. This lack of tissue is also consistent with bleeding from an atrophic endometrium, which is a benign condition. When endometrium is present, a wide range of histology can be observed. Occasionally, simple proliferative endometrium is found. The endometrium can exhibit simple hyperplasia, more marked adenomatous hyperplasia, or hyperplasia with atypical cells, resulting in a diagnosis of atypical endometrial hyperplasia.
Endometrial hyperplasia requires a more aggressive workup. Atypical adenomatous endometrial hyperplasia is considered by most to be the equivalent of an intraepithelial malignancy, and hysterectomy is often advised.
Hormone-induced postmenopausal uterine bleeding can be the result of endogenous or exogenous hormonal effects. The proliferation of endometrium in a patient who is not receiving exogenous hormonal therapy is generally attributed to endogenous production of estrone. Estrone is the peripheral conversion product of the weak androgenic precursor androstenedione (85% from adrenal, 15% from ovary), and its synthesis occurs primarily in adipose tissue. In the absence of exogenous hormonal therapy, one must also exclude the possibility of an estrogen-producing ovarian tumour (granulosis cell tumor).
The most important point about the significance of postmenopausal bleeding is its frequent association with gyaecological malignancy, particularly endometrial carcinoma. Although the incidence of malignancy to explain postmenopausal bleeding has decreased in recent decades, diagnostic efforts must carefully consider and rule out possible malignancy by use of appropriate diagnostic procedures, especially careful pelvic examination and uterine curettage. One must remember always that an endometrial office biopsy is helpful for the diagnosis of suspected endometrial carcinoma only if the biopsy is positive. |
| BEST SURGICAL PRACTICES FOR STUDY OF POSTMENOPAUSAL ENDOMETRIUM |
- Endometrial sampling can be done by probet cannula or 10 FG cannula and syringe in office practice. Four quadrant endometrial sampling biopsy, or formal dilatation and curettage (D&C), all of these techniques can miss significant lesions, and the concurrent use of vaginal ultrasonography or SIS will improve sensitivity.
- Although hysteroscopy is the gold standard for evaluating endometrial cavity pathology, saline infusion sonography (SIS) has comparable sensitivity and is less invasive and less expensive.
- Hysteroscopy is a valuable adjunct to D&C, particularly in the patient at higher risk for focal endometrial pathology that might be missed on endometrial sampling.
- Biopsy under ultrasound guidance may reduce the risk of complication such as perforation during difficult cervical D&C, such as in the stenotic postmenopausal patient or in the case of a large uterus.
|
|
|
|


